Retinal Neovascularization: Mechanisms and Treatment Approaches
Originally published by Palmetto Retina Center
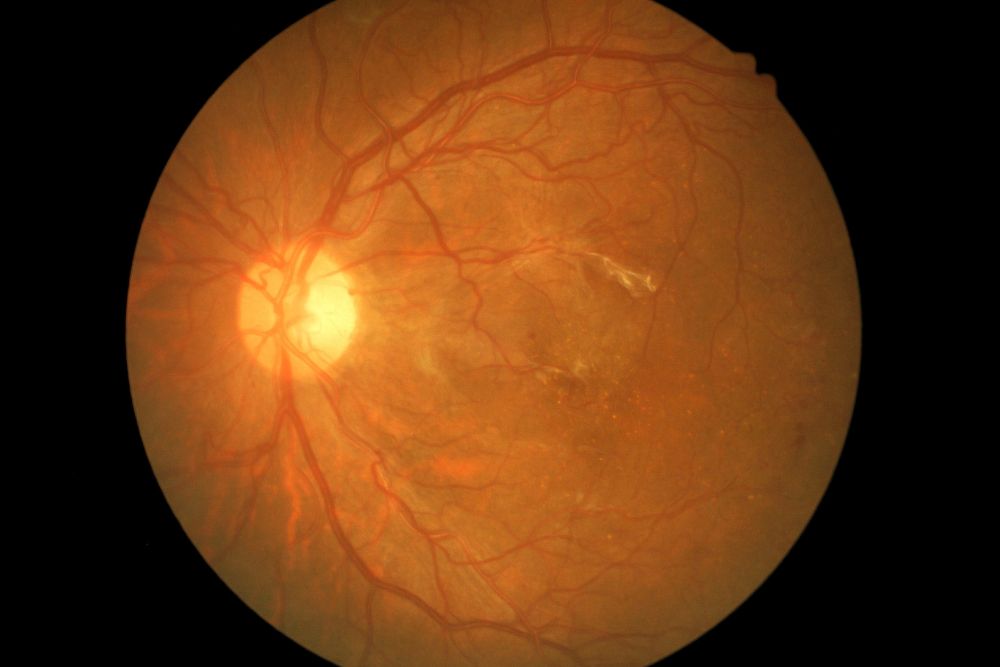
Neovascularization, a common and serious characteristic of several retinal conditions, involves the development of new blood vessels to compensate for those lost due to injuries or underlying conditions. These new vessels are fragile and prone to breaking, allowing fluid and blood to seep into the retina and its surrounding areas. It is essential to monitor your vision and have regular comprehensive, dilated eye exams. This allows your ophthalmologist to diagnose the underlying condition earlier and initiate appropriate treatments, such as intravitreal injections or other therapies.
Retinal Conditions Involving Neovascularization
Wet Age-Related Macular Degeneration (AMD)
Age-related macular degeneration (AMD) is the leading cause of vision loss in individuals over 50. It occurs due to the gradual deterioration of the macula – the central part of the retina responsible for straight-ahead vision and performing close-up tasks. In the advanced stage known as wet (or exudative) AMD, the primary symptom is choroidal neovascularization (CNV). This condition affects the choroid, a spongy, pigmented layer of blood vessels and connective tissue that supplies essential oxygen and blood to the outer layers of the retina.
Diabetic Retinopathy
Diabetes causes chronic high blood glucose that gradually weakens the retina’s tiny blood vessels. Neovascularization is specific to the more advanced form, proliferative diabetic retinopathy (PDR). You may also experience a condition called diabetic macular edema, which is swelling of the macula that occurs as fluid or blood accumulates. Macular fluid leakage may increase risks for conditions like retinal detachment, and central vision loss, permanent retinal nerve damage, and blindness may occur.
Retinal Detachment
Neovascularization can result in excessive blood and fluid leaking into the eye’s vitreous, which is the clear, gel-like substance that fills the eye. The excess fluids can pull on the retina, leading to a partial or full retinal detachment, a condition requiring immediate medical attention. Neovascularization is typically associated with tractional retina detachment, which may occur due to diabetes, surgery, or fluid accumulation.
Retinal Artery and Vein Occlusions
Retinal artery and vein occlusions are serious eye conditions that can lead to vision loss. They occur when there is a blockage in the small blood vessels (arteries or veins) that supply the retina. Neovascularization can occur when these occlusions impede the eye’s regular circulation.
Neovascularization Treatment Options
Intravitreal Injections
Neovascularization treatment may vary depending on the cause, but the standard of care is intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF). They inhibit protein development, either by slowing abnormal blood vessel growth or preventing blood vessels from leaking fluid in the eye. Anti-VEGF medications include Avastin® (bevacizumab), Beovu® (brolucizumab), Eylea® (aflibercept), Lucentis® (ranibizumab), and Vabysmo® (faricimab-svoa).
Laser Therapies
Your retina specialist may also perform laser treatment to safely remove unusual blood vessels and tissue. The main technique, pan-retinal photocoagulation (PRP), often used for diabetic retinopathy and retinal vein occlusions, is administered to the peripheral retina. Photodynamic therapy, combining light and medications, eradicates tissue and blocks vessel growth. With a thermal laser, common with wet AMD, a hot laser burns blood vessels and prevents additional growth.
Vitreoretinal Surgery
Should surgery be needed, you may undergo a vitrectomy, involving partial or complete vitreous removal from the back of the eye. It’s performed for advanced diabetic retinopathy cases when eye scarring has developed. With pneumatic retinopexy, often used for retinal detachment, a gas bubble is injected into the vitreous, sealing breaks until the retina reattaches. Techniques like photocoagulation or cryotherapy (freezing) may also be conducted.
Explore Retinal Neovascularization and Treatment Approaches
Neovascularization can cause serious symptoms and threaten vision, making it crucial to know its signs and see a retina specialist for a quick diagnosis. If you’re at risk for any of these conditions, we encourage you to find a Retina Consultants of America doctor near you and schedule an appointment with one of our retina specialist